Proteinuria (Prtn)
Proteinuria (Prtn) : Understanding Its Significance and Implications
Definition:
Proteinuria (Prtn) is the presence of excess protein in the urine, which can be an indicator of kidney damage or disease. Normally, urine contains very little protein, as healthy kidneys filter waste products while retaining essential proteins in the bloodstream. When the kidneys are damaged or diseased, they may allow proteins to leak into the urine.
Causes of Proteinuria
Proteinuria can result from a variety of conditions, including:
- Overview: CKD is characterized by a gradual loss of kidney function over time, often leading to proteinuria as the kidneys become less effective at filtering waste.
- Impact: Persistent proteinuria in CKD is associated with disease progression and increased cardiovascular risk.
- Overview: Diabetes can lead to diabetic nephropathy, a condition where high blood sugar levels damage the kidneys’ filtering units.
- Impact: Proteinuria is often one of the first signs of kidney damage in diabetic patients.
Hypertension:
- Overview: High blood pressure can cause damage to the blood vessels in the kidneys, leading to protein leakage.
- Impact: Hypertensive nephropathy may result in significant proteinuria and further kidney impairment.
- Overview: This group of diseases involves inflammation of the glomeruli, which can disrupt normal kidney function and result in proteinuria.
- Impact: Depending on the severity and type, glomerulonephritis can lead to acute or chronic kidney failure.
Infections:
- Overview: Certain infections, particularly urinary tract infections (UTIs) and systemic infections, can temporarily increase protein levels in urine.
- Impact: While often reversible, persistent infections may indicate underlying kidney issues.
Mechanism of Action
The presence of protein in urine typically indicates a disruption in the filtration barrier of the kidneys:
- Glomerular Damage: Damage to the glomeruli allows larger proteins (such as albumin) to escape into the urine.
- Tubular Dysfunction: In some cases, tubular damage can also contribute to proteinuria by impairing reabsorption processes.
Clinical Implications
Proteinuria is an important clinical marker that can indicate:
- Kidney Disease Progression: Persistent proteinuria is associated with a higher risk of progression to end-stage renal disease (ESRD).
- Cardiovascular Risk: Patients with proteinuria are at increased risk for cardiovascular events due to underlying kidney dysfunction.
- Monitoring Treatment Efficacy: Changes in levels of proteinuria can help assess the effectiveness of treatments for underlying conditions like diabetes or hypertension.
Diagnosis and Management
Diagnosis:
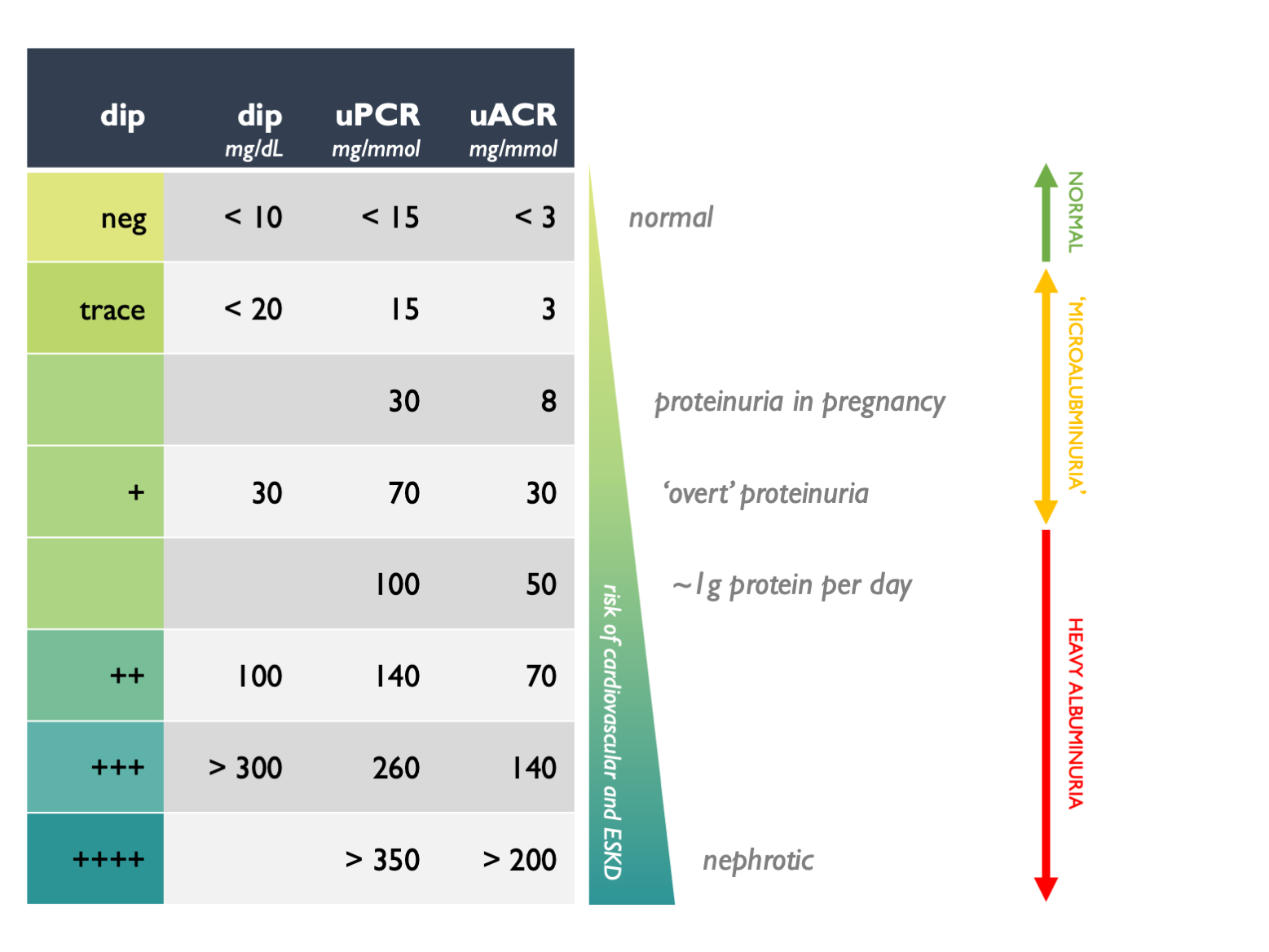
- Urinalysis: A routine urinalysis can detect protein levels; further tests may include a 24-hour urine collection or urine protein-to-creatinine ratio.
- Blood Tests: Assessing kidney function through serum creatinine and blood urea nitrogen (BUN) levels is essential.
Management:
- Addressing Underlying Conditions: Effective management of diabetes and hypertension is crucial for reducing proteinuria.
- Medications: Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are often prescribed to reduce protein leakage and protect kidney function.
- Lifestyle Modifications: Dietary changes, weight management, and regular exercise can help control conditions contributing to proteinuria.
Conclusion
Proteinuria is a significant clinical finding that serves as an important indicator of kidney health and overall systemic conditions. Early detection and management are vital for preventing progression to more severe renal impairment and associated complications.
Consult with Our Team of Experts Now!
At DrStemCellsThailand‘s Anti-Aging and Regenerative Medicine Center of Thailand, we specialize in comprehensive care for patients with kidney-related issues, including those experiencing proteinuria. Our team focuses on innovative therapies aimed at improving kidney function and overall health. If you or a loved one is facing renal challenges, consult with our experts today to explore personalized treatment options that could enhance your quality of life!
Consult with Our Team of Experts Now!
References
- Levey AS et al. “Chronic Kidney Disease.” The Lancet. 2011; 377(9769): 2089-2100. DOI: 10.1016/S0140-6736(11)60178-5.
- KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney International Supplements. 2014; 3(1): 1-150. DOI: 10.1016/j.kisu.2013.10.002.
- Mottl AK et al. “Proteinuria: A Marker for Kidney Disease.” American Family Physician. 2015; 92(11): 935-940. Available at: AAFP.














