Post-Inflammatory Hypopigmentation (PIH)
Post-Inflammatory Hypopigmentation (PIH): Causes and Treatment
What is PIH?
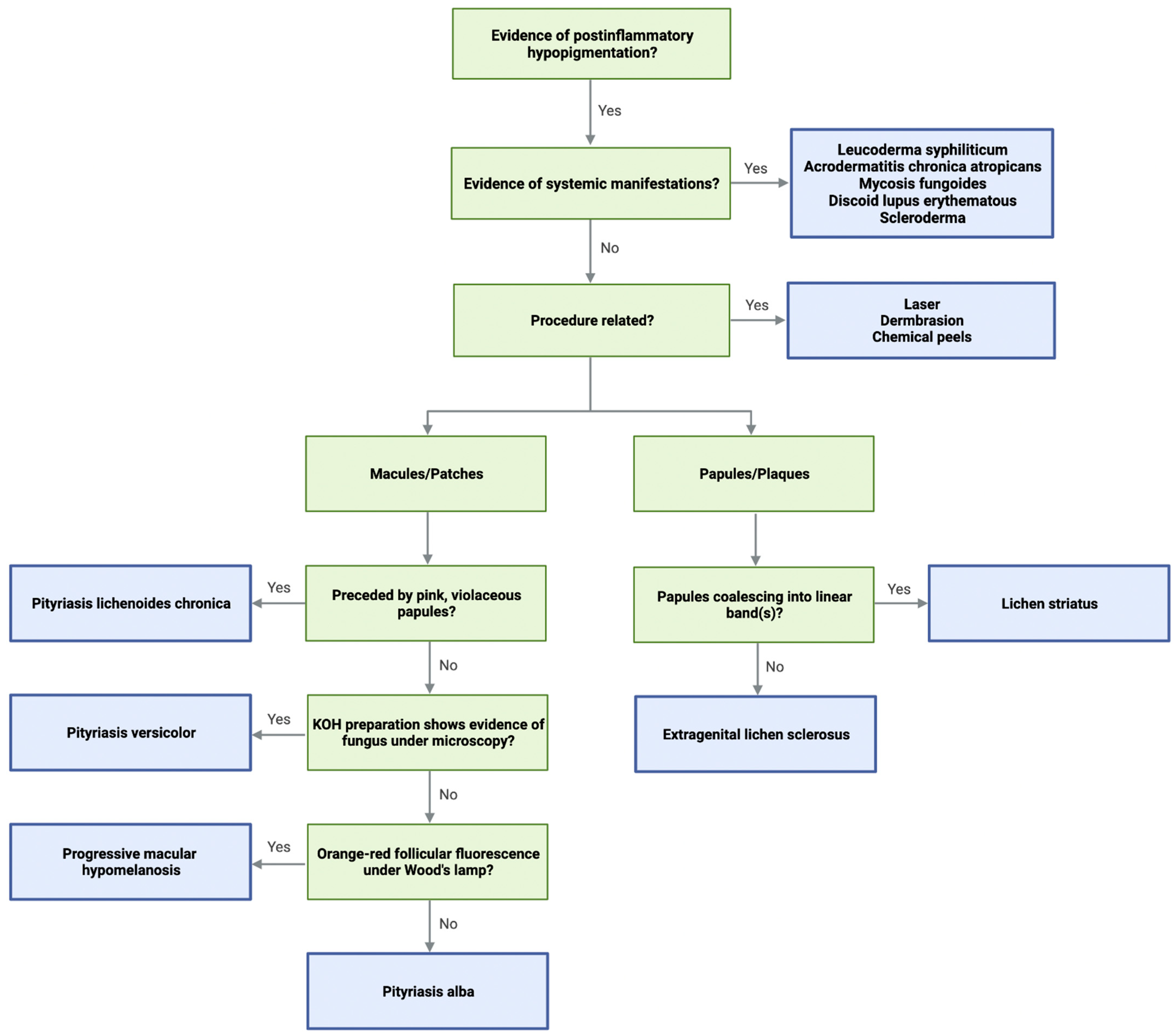
Post-inflammatory hypopigmentation (PIH) is a skin condition where lighter patches develop following inflammation or injury to the skin. It results from reduced melanin production, impaired melanosome transfer, or damage to melanocytes caused by prior inflammatory or infectious processes.
Causes
- Inflammatory skin diseases like eczema, psoriasis, discoid lupus erythematosus, and lichen planus.
- Infectious skin conditions such as pityriasis versicolor, fungal infections, or cutaneous infections.
- Dermatologic procedures including laser therapy, chemical peels, or vigorous skin trauma leading to melanocyte injury.
- UV exposure can worsen hypopigmentation.
- In some diseases like scleroderma and progressive macular hypomelanosis, melanocyte destruction causes long-lasting hypopigmentation.
Pathophysiology
- Melanocyte dysfunction or destruction decreases melanin synthesis.
- Disrupted melanosome transfer to keratinocytes.
- Inflammatory cytokines, oxidative stress, and vascular mediators contribute to pigment loss.
Treatment Options
- Address underlying causes: Control inflammation or infection with topical corticosteroids, antifungals, or antibiotics as appropriate.
- Phototherapy: Narrowband UVB (nbUVB) and excimer laser can stimulate melanocyte proliferation and pigment production, especially in conditions like vitiligo or lichen planus.
- Topical Immunomodulators: Tacrolimus can promote repigmentation by enhancing melanocyte migration and melanin synthesis.
- Prostaglandin analogs: Bimatoprost may encourage melanocyte activation and pigment restoration.
- Sun Protection: Broad-spectrum sunscreen prevents further pigment loss and protects sensitive areas.
- Laser-assisted drug delivery: Enhances topical treatment penetration and efficacy.
Prognosis and Considerations
- Some cases resolve spontaneously over months as inflammation subsides.
- Treatment response varies by severity and cause; combination therapy is often needed.
- Early intervention can improve outcomes and reduce disease chronicity.
- Patient expectations should be managed regarding treatment duration and results.
Summary
Post-inflammatory hypopigmentation results from inflammation-induced melanocyte loss or dysfunction. Successful management involves treating underlying conditions, phototherapy, topical immunomodulators, and sun protection to stimulate repigmentation and restore skin tone.
Consult with Our Team of Experts Now!
For individualized assessment and tailored treatment strategies for post-inflammatory hypopigmentation, consult with our dermatology specialists who integrate the latest evidence-based therapies.
References:
- Deshmukh P, Narayanan V. Post-Inflammatory Hypopigmentation: Review of the Etiology, Clinical Features, and Treatment Approaches. Clin Exp Dermatol. 2023 Feb;48(2):237-245. doi:10.1111/ced.15056. Available at: https://pubmed.ncbi.nlm.nih.gov/36769891/
- Herbert AA, Goh J, Sterling JC. Postinflammatory Hypopigmentation: Pathophysiology and Therapeutic Options. J Eur Acad Dermatol Venereol. 2011 Jun;25(6):641-648. doi:10.1111/j.1468-3083.2010.04088.x. Available at: https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2230.2011.04088.x
- Dermatology Times. Treating and Preventing Postinflammatory Hypo- and Hyperpigmentation. 2023 Aug 10. Available at: https://www.dermatologytimes.com/view/treating-and-preventing-postinflammatory-hypo–and-hyperpigmentation















