Fatty Liver Disease (Steatosis): Understanding the Condition
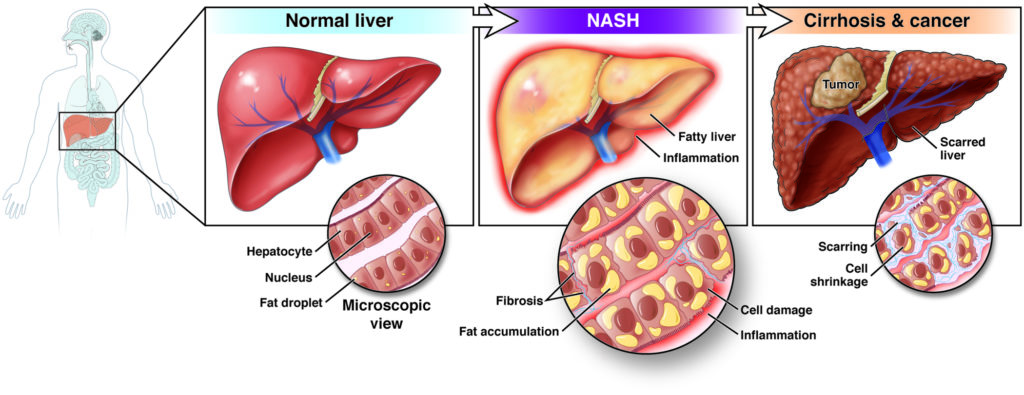
Fatty Liver Disease (Steatosis), also known as hepatic steatosis or steatotic liver disease (SLD), is a common condition characterized by the accumulation of excess fat in the liver cells238. There are two main types5:
- Nonalcoholic fatty liver disease (NAFLD)15
- Alcoholic fatty liver disease, also called alcoholic steatohepatitis5
NAFLD is further categorized into simple fatty liver (hepatic steatosis), and nonalcoholic steatohepatitis (NASH), the more advanced form35.
Symptoms of Fatty Liver Disease (Steatosis)
Often, fatty liver disease presents no symptoms, and people are unaware they have it until it’s discovered during liver function tests for other conditions134. However, some may experience134:
If the condition progresses to NASH or cirrhosis, more severe symptoms can occur136:
- Abdominal swelling (ascites)136
- Enlarged blood vessels under the skin36
- Larger-than-normal breasts in men36
- Red palms13
- Yellowing of the skin and eyes (jaundice)136
- Itchy skin146
- Nausea36
- Weight loss or loss of appetite36
- Mental confusion36
- Dark-colored urine6
- Pale stools6
- Swollen legs (edema)146
Causes and Risk Factors
Fatty liver disease results from excess fat buildup in the liver2. Specific causes and risk factors vary between the two main types235:
- NAFLD: Linked to genetics, obesity, insulin resistance, type 2 diabetes, high blood sugar (hyperglycemia), and high levels of fats (especially triglycerides) in the blood1.
- Alcoholic Fatty Liver Disease: Caused by heavy alcohol use, as the liver breaks down alcohol and generates harmful substances that damage liver cells5.
Additional risk factors include2:
- Metabolic syndrome (obesity, high blood pressure, abnormal cholesterol levels, insulin resistance)2
- Family history of fatty liver disease or obesity1
- Growth hormone deficiency1
- Rapid weight loss and malnutrition2
- Certain infections3
- Drug toxicity3
Diagnosis of Fatty Liver Disease
Because there are often no symptoms, fatty liver disease is commonly diagnosed during tests for other conditions4. Doctors may use the following3:
- Physical exam
- Blood tests (liver function tests)3
- Imaging tests, such as ultrasound, CT scan, or MRI3
- Liver biopsy3
Prevention
There are several ways to prevent or manage fatty liver disease4:
- Maintain a healthy weight4
- Eat a balanced diet4
- Exercise regularly4
- Limit or avoid alcohol4
- Control blood sugar, cholesterol, and triglyceride levels4
Consult with Our Team of Experts Now!
At DrStemCellsThailand (DRSCT)‘s Anti-Aging and Regenerative Medicine Center of Thailand, we emphasize comprehensive evaluations and personalized treatment plans of Cellular Therapy and Stem Cells for managing various health conditions. If you have questions about fatty liver disease or would like more information on our services related to liver health, consult with our experts today!
Consult with Our Team of Experts Now!
References:
- Pathophysiology of Non-Alcoholic Fatty Liver Disease: This article reviews the current knowledge on the dynamics of major circulating effectors/mediators of fatty liver, such as circulating lipids, released compounds from adipose, muscle and liver tissues and pancreatic and gut hormones in relation to lifestyle (i.e., diet and exercise) and inflammation. DOI: Not Available. Visit: https://pmc.ncbi.nlm.nih.gov/articles/PMC5187882/
- New insights into the pathophysiology of nonalcoholic fatty liver: This article analyzes new factors associated with the main theories on the pathophysiology of NAFLD are analyzed. During the insulin resistant state, the liver adapts by increasing MTP expression via nuclear localization of the forkhead box-containing protein O subfamily-1 (FoxO1) and inducing MTP transcription. DOI: Not Available. Visit: https://www.elsevier.es/en-revista-annals-hepatology-16-articulo-new-insights-into-pathophysiology-nonalcoholic-S1665268119318216
- Pathophysiology and Mechanisms of Nonalcoholic Fatty Liver Disease: This review covers the evolving concepts of NAFLD from both human and animal studies. The review also discuss recent clinical and diagnostic methods assessing NAFLD diagnosis, progression, and outcomes; compare the features of genetic and dietary animal models of NAFLD; and highlight pharmacological approaches for disease treatment. DOI: https://www.annualreviews.org/doi/10.1146/annurev-physiol-021115-105331















