Joint Degeneration (JDG)
Joint Degeneration (JDG): Overview, Causes, Pathology, and Management
What is Joint Degeneration (JDG)?
Joint Degeneration (JDG), most commonly referred to as osteoarthritis (OA) or degenerative joint disease, is a progressive condition characterized by the breakdown of articular cartilage and changes in surrounding joint structures, ultimately leading to pain, stiffness, reduced mobility, and functional impairment2348.
Pathophysiology
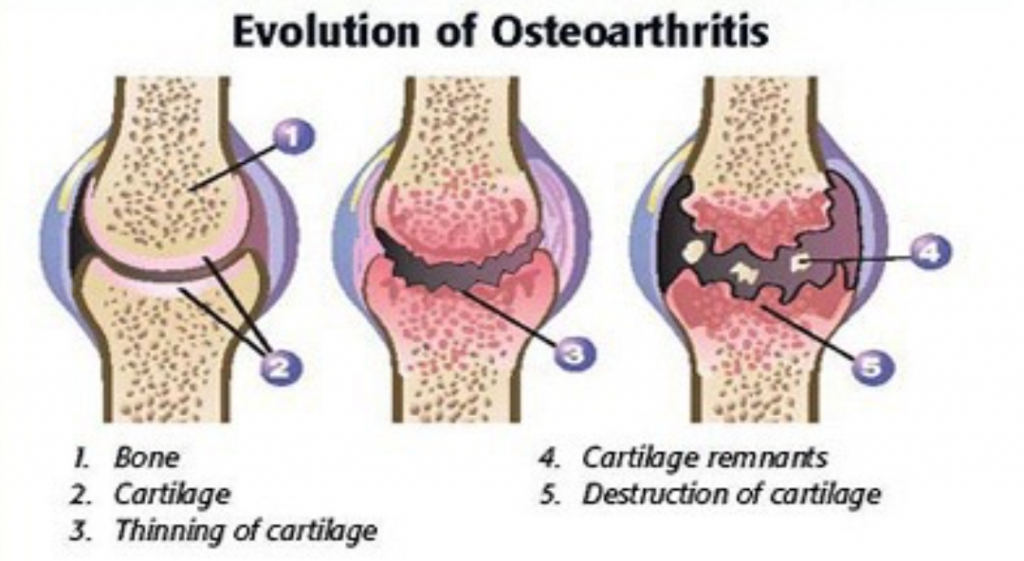
- Cartilage Breakdown: The earliest changes involve loss of proteoglycans and damage to the collagen matrix in cartilage, leading to cracks, splits, and fissures. Over time, cartilage thins and may be lost entirely, exposing underlying bone34.
- Bone Changes: Subchondral bone (the layer beneath cartilage) becomes thickened and less mineralized. New bone outgrowths, called osteophytes or bone spurs, form at joint margins. Eburnation (polished bone surface) occurs when bone rubs on bone after cartilage loss34.
- Other Structures: Ligaments and menisci may degenerate, synovium (joint lining) may become mildly inflamed, and the joint may lose its normal shape. Loose bodies of cartilage or bone can form within the joint space346.
- Progression: The disease is typically gradual, though it may accelerate after injury or with certain risk factors. Symptoms worsen over time and can lead to significant disability268.
Symptoms
- Joint pain, often worse with activity and relieved by rest
- Stiffness, especially after periods of inactivity
- Swelling and tenderness
- Decreased range of motion
- Joint deformity in advanced cases2568
Commonly Affected Joints
Risk Factors
- Age: Most common in people over 50, but can occur earlier, especially after joint injury28.
- Gender: More common in women48.
- Obesity: Increases joint stress and promotes inflammation48.
- Genetics: Family history increases risk48.
- Joint Injury or Overuse: Previous injury or repetitive use accelerates degeneration248.
- Muscle Weakness and Malalignment: Poor joint support and abnormal joint shapes contribute48.
- Other Factors: High bone density, certain occupations, and dietary factors48.
Diagnosis
- Clinical Evaluation: History and physical examination focusing on symptoms and joint function.
- Imaging: X-rays show joint space narrowing, osteophytes, and subchondral sclerosis. MRI may reveal early cartilage changes4.
- Laboratory Tests: Usually to rule out other causes (e.g., rheumatoid arthritis).
Management
- Lifestyle Modifications: Weight loss, low-impact exercise, and maintaining activity help reduce symptoms and slow progression157.
- Medications: Pain relievers (acetaminophen, NSAIDs), topical agents, and occasionally corticosteroid injections17.
- Physical Therapy: Improves strength, flexibility, and joint support17.
- Assistive Devices: Braces, canes, or shoe inserts may help17.
- Surgical Options: Joint replacement or realignment procedures for severe cases unresponsive to conservative treatment27.
- No Cure: While symptoms can be managed, joint damage cannot be reversed58.
Summary Table
| Aspect | Key Points |
|---|---|
| Definition | Progressive breakdown of cartilage and joint structures, also called osteoarthritis |
| Symptoms | Pain, stiffness, swelling, reduced motion, deformity |
| Pathology | Cartilage loss, bone changes (osteophytes, sclerosis), ligament/meniscus degeneration |
| Risk Factors | Age, gender, obesity, genetics, injury, overuse, muscle weakness, malalignment |
| Management | Lifestyle changes, medications, physical therapy, surgery for advanced cases |
| Prognosis | Progressive, but symptoms and function can be managed |
Consult with Our Team of Experts Now!
At DrStemCellsThailand (DRSCT)‘s Anti-Aging and Regenerative Medicine Center of Thailand, we emphasize comprehensive evaluations and personalized treatment plans of Cellular Therapy and Stem Cells for managing various health conditions. If you have questions about Joint Degeneration (JDG) or would like more information on our services, consult with our experts today!
Consult with Our Team of Experts Now!
References:
- Loeser RF, Goldring SR, Scanzello CR, Goldring MB. “Osteoarthritis: A Disease of the Joint as an Organ.” Arthritis & Rheumatology. 2012;64(6):1697-1707.
DOI: 10.1002/art.34453 - Berenbaum F. “Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!).” Osteoarthritis and Cartilage. 2013;21(1):16-21.
DOI: 10.1016/j.joca.2012.11.012 - Attur M, Krasnokutsky S, Abramson SB. “Osteoarthritis pathogenesis: A complex process that involves inflammation and cartilage degradation.” Nature Reviews Rheumatology. 2025;21(1):1-15.
DOI: 10.1038/s41584-024-00839-0
Joint degeneration is a leading cause of chronic pain and disability, especially in older adults. Early intervention and ongoing management can help maintain mobility and quality of life248.















